指定論文與版權
新思惟的「臨床研究與發表」工作坊,使用 吳昭慶醫師 已發表的研究,作為 課程指定論文。
多數國際期刊規範,論文的文字與圖片,屬於原作者,但「排版後」的論文,版權屬於雜誌社。所以,不管是教學或商業使用,散佈下載的論文 PDF,並不在授權範圍內,也就是說,我們過去有時候,直接把論文 PDF 寄給同事參考,這動作事實上是「違法」的。
新思惟國際,尊重各種形式的智慧財。所以,經吳昭慶醫師同意後,取得論文的 MS-Word 版本原稿,委請設計師,用不同的風格,重新排版過。版權由「新思惟國際」回贈給吳昭慶醫師,並均能獨立使用。
這份論文,將作為這次工作坊的教材。
Arthroplasty vs. ACDF (two levels) by Jau-Ching Wu, MD, PhD
論文故事
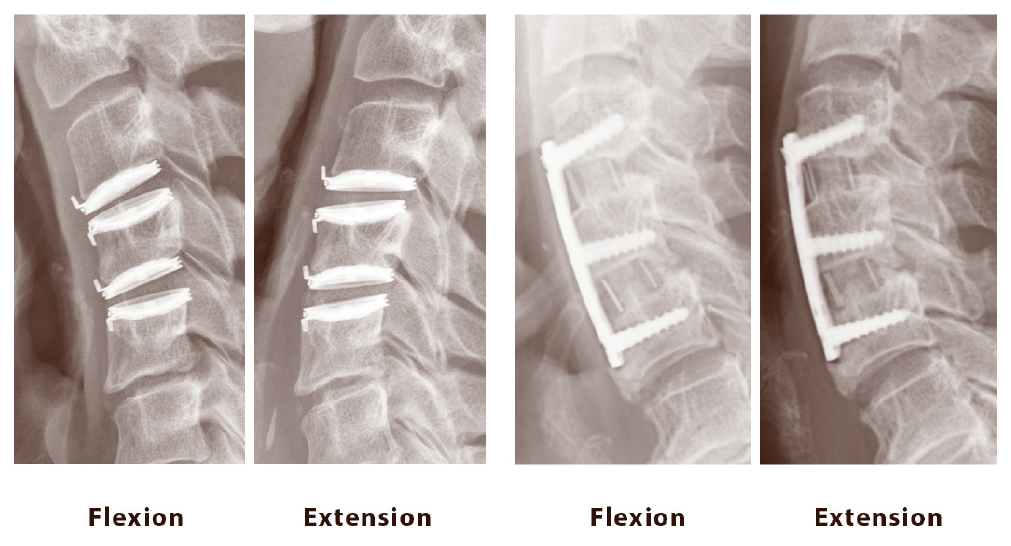
人類的頸椎,會因為姿勢不良或外傷而退化。如果椎間盤突出,產生神經症狀,復健無效,就需要開刀。目前開刀的主流方法,是從前面開,拿掉退化的椎間盤,作減壓,接著打上金屬板固定,避免不穩定的晃動。這個手術,叫做 anterior cervical discectomy and fusion (ACDF)。
「單節」的 ACDF 手術,會使頸椎活動範圍減少 7 度,根據 FDA-IDE trial,如果改放「人工椎間盤」,就不會有這樣的問題,且手術一樣安全有效。
不過臨床上,「連續兩節」頸椎都需要手術的患者,並不在少數,卻沒有人研究過,連續兩節「人工椎間盤」置放,對比於連續兩節的 ACDF 手術,是否一樣有效安全,且能保留活動範圍。於是,吳昭慶醫師預計用臨床研究,回答這個問題。
後續的故事,就請各位自行閱讀全文囉。
引用
Fay LY, Huang WC, Tsai TY, Wu JC, Ko CC, Tu TH, Wu CL, Cheng H. Differences between arthroplasty and anterior cervical fusion in two-level cervical degenerative disc disease. Eur Spine J. 2014 Mar; 23(3):627-634. doi: 10.1007/s00586-013-3123-8.
摘要
PURPOSE: Although arthroplasty is an accepted option for two-level disease, there is a paucity of data regarding outcomes of two-level cervical arthroplasty. The current study was designed to determine differences between two-level cervical arthroplasty and anterior fusion.
METHODS: Seventy-seven consecutive patients who underwent two-level anterior cervical operations for degenerative disc disease were divided into the arthroplasty (37 patients) and fusion (40 patients) groups. Clinical outcomes were measured by Visual Analogue Scale (VAS) of neck and arm pain, Japanese Orthopedic Association (JOA) scores, and Neck Disability Index (NDI). Every patient was evaluated by radiography and computed tomography for fusion or detection of heterotopic ossification.
RESULTS: Thirty-seven patients (with 74 levels of Bryan discs) were compared with 40 patients who had two-level anterior fusion (mean follow-up of 39.6 ± 6.7 months). There was no difference in sex, but the mean age of the arthroplasty group was significantly younger (52.1 ± 9.1 vs. 63.0 ± 10.6 years, p < 0.001). The mean estimated blood loss was similar (p = 0.135), but the mean operation time was longer in the arthroplasty group (315.5 ± 82.0 versus 224.9 ± 61.8 min, p < 0.001). At 24 months post-operation, the arthroplasty group had increased their range of motion than pre-operation (23.5° versus 20.1°, p = 0.018). There were significant improvements in neck or arm VAS, JOA scores, and NDI in both groups. However, there were no differences in clinical outcomes or adverse events between the two groups.
CONCLUSIONS: Clinical outcomes of two-level arthroplasty and anterior cervical fusion are similar 39.6 months after surgery. Cervical arthroplasty preserves mobility at the index levels without increased adverse effects.
最新活動
